U.S. Opioid Crisis Calls for Fewer Prescriptions
Due to the opioid addiction epidemic, doctors should reconsider prescriptions.
PHOTO | Tribune News Service
The opioid crisis in America is the worst it has ever been and shows no signs of slowing down.
From Tom Petty to Prince, opioid deaths have been featured in the media more and more. And it isn’t only celebrities who are being affected. Every day more than 90 Americans die of an opioid overdose, relating to both prescription and non-prescription opioid consumption, according to the National Institute on Drug Abuse.
The solution lies in the extreme reduction of the use of prescription opioids.In order to get to the root of the problem, it is necessary to look at how the crisis first started.
In the ‘90s, pharmaceutical companies told the public that opioid medications (morphine, oxycodone, Percocet, Vicodin. etc.) were safe and effective treatment options. Since then, the prescription of opioids for chronic pain has nearly quadrupled, according to the Center for Disease Control. Today, opioids are the “standard of the world” when it comes to treatment of severe and chronic pain, according to the U.S. National Library of Medicine. It is true that opioids are an effective treatment, but it is also true that they are overprescribed.
Around 20 percent of people diagnosed with non-cancer or pain-related diseases are given opioid prescriptions, according to the CDC. Despite the dramatic increase in opioid prescriptions, there is no reported increase in Americans who suffer from pain related diseases. This increase in prescription has led to an increase in opioid dependency.
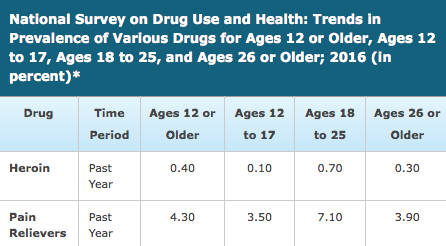
With the increase in prescription opioid use came an increase in non-prescription opioid use and prescription abuse according to the US NLM. According to the National Survey on Drug Use and Health, first-time abusers of prescription opioids rose from 628,000 in 1990 to 2.4 million in 2004 and visits to the emergency room for reasons involving prescription opioid abuse increased by 45 percent between 2000 and 2002 alone. These statistics don’t even account for overdoses.
Nearly 100 million Americans suffer from chronic pain and many rely on opioid medication to get through their day. This demographic is often used as a reason why doctors shouldn’t decrease opioid use. However, the patients are not the problem. Rather, it is the doctors who are overambitious and generous when it comes to prescribing opioids and who often earn extra with the prescriptions they give.
One in 12 doctors receive some sort of extra payment from opioid companies, according to Boston Medical Center. These benefits range from something as small as a free lunch to an actual cash payment. In all, tens of millions of dollars are spent marketing opioids to doctors. On top of monetary benefits, many doctors haven’t been trained in chronic pain or addiction. According to Harvard Health Publishing, doctors have little training in “safely prescribing pain medications, recognize patients at high risk for overdose, intervening when patients need to be taken off of opioids, and adequately treat opioid addiction.”
Over the counter, Acetaminophen, found in Tylenol, is the recommended first treatment for pain by the American College of Rheumatology. If a stronger dosage is needed Nonsteroidal Anti-Inflammatory Drugs are available in weaker over the counter doses or in higher prescription doses. Other options include corticosteroids, Serotonin and Norepinephrine Reuptake Inhibitors or even just exercise. Despite these proven solutions, doctors still turn to opioids first.
Only when doctors begin to lower their opioid prescriptions will the opioid crisis improve.